Kettlebells. Do they have a role in the clinical setting? Should they be used in a rehabilitation for patients in the outpatient physical therapy clinic? This is a burning question that has not been sufficiently answered. Kettlebells do have a role, but certain things must be considered before any clinician dares to bring kettlebells into the clinic. Below are the key concepts that clinicians need to know.
The Backstory
Chuck and I went through the Master’s Degree program for Physical Therapy at the University Of Maryland School of Medicine. We both had our unique backgrounds and passions for strength training, even back then. Since that time, we’ve also come to realize how little we actually knew about the proper applications of strength and movement, especially as it pertains to patients in the outpatient physical therapy setting.
While I’m a ‘former’ physical therapist, these days I’m a strength coach and teacher of movement. I’ve learned a lot about the principles of strength since my days being in the clinic as a PT. The truth is that my journey really began when I discovered kettlebells and was introduced to the methods and techniques taught by Pavel. Although I’m no longer a practicing clinician, there’s no doubt that kettlebells would have been part of my clinical approach had I known then what I know today.
Chuck, on the other hand, is still a practicing physical therapist who actively uses kettlebells in the clinics he oversees. We’ve had many conversations about using kettlebells in the clinic, which is the genesis of this article. He uses kettlebells as a standard component of his rehabilitation process and also teaches the methods and techniques to other clinicians he works with.
Recently we decided to have an in-depth discussion about the roles and limitations. Here’s the conversation between Chuck and I with several actionable takeaways and perspectives for the clinician to understand.
Intro to the “Deep Dive” Conversation
Scott: I’ve treated many orthopedic patients during my years as a clinician. While I don’t practice in the clinical setting today, I’ve thought a lot about how I would have used kettlebells in my approach to rehabilitation.
Obviously, this is dependent on the patient and the diagnosis that you’re dealing with. But had I known about the unique benefit of kettlebells, it could have been the difference-maker in my approach.
For example, the get-up (or components of the get-up) could have been great for teaching movement patterns for spine and shoulder patients.
After learning an unloaded get-up pattern, a kettlebell could then be introduced and would be an appropriate tool to progress with, in terms of movement and strength.
A proper hip hinge: a kettlebell deadlift would have been a highly-utilized tool for this movement pattern.

Certainly, carries and different variations such as a bottom’s-up carry, come immediately to mind. We know from the work of Dr. Stuart McGill that the core musculature is highly active with bottom’s-up kettlebell carries. Carries are self-regulating exercises and easy to learn.
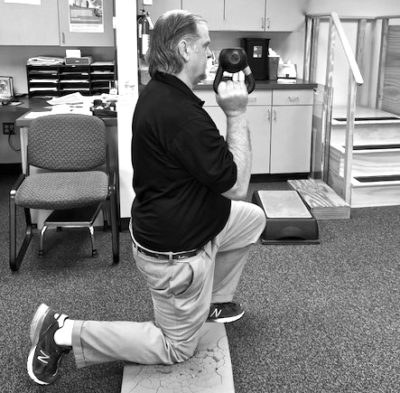
The kettlebell is also a very unique tool for pressing. I think it’s the best tool for pressing and there are many pressing variations, such as half-kneeling and tall-kneeling that would be very applicable, relevant, and useful in the clinical setting. These are just a few examples that come to mind.
Chuck: Being a physical therapist for 22 years now, I’ve continually searched for the answer to the big question, how do you really get people stronger?
When I came across kettlebells over 12 years ago, it became the perfect tool for strength training. I have only worked in the outpatient physical therapy setting where we see everybody from ankle sprains to post-surgical patients. The majority of the patients I see come to physical therapy in the outpatient setting with mechanical cervical (neck) and lumbar (back) spinal impairments.
Over time, I have integrated the kettlebell concepts into my practice. I like to keep these concepts simple for the clinicians—and for the patients.
These concepts can be summarized with these 3 points:
- Can you create tension?
- Can you hinge from the hips?
- Can you breathe diaphragmatically?
Many of our patients lack strength and mobility. Tension is something that could be viewed as a bad thing for the patients. What I mean is that the majority of our patients experience upper trap tension due to sitting for 13 hours a day and consistently looking down at their computers or an electronic device. The creates lot of problems from increased pain (neck, shoulder and back), the inability to get off the floor, and even trouble getting up from a chair.
We can use these 3 concepts (tension, hip hinge and breathing) and apply them to a simple task like getting up out of chair.
We teach patients how to hinge from the hips, drive (root) their feet into the ground, and create tension as they stand up by squeezing their glutes and fists. I make this even more simple and call it “Grip-Butt-Squeeze.” They do this with diaphragmatic inhalation and exhalation as the patient stands. It’s really that simple.
You would be amazed how many patients can’t get out of a chair without experiencing knee pain or needing assistance from their arms. However, using these 3 simple concepts and practicing the skill every time a patient gets out of a chair, and the patient gains strength and confidence with their daily activities.
Most patients do not know how to flex from their hips, so teaching someone how to hinge is major in decreasing low back pain and creating functional movement patterns that apply to their daily activities.
Another important concept would be to teach the patient how to breathe correctly. As you know, everything starts with good breathing. We spend a lot of time in the clinic teaching the patients how to perform diaphragmatic breathing. One of my therapists calls breathing practice “belly time” as the patient assumes the prone position and focuses on breathing diaphragmatically for 5 minutes.
These are the 3 simple concepts I teach my clinicians and patients to improve their strength.
Now, the Questions
Scott: What’s the most important factor for using kettlebells safely in the clinic and maximizing their effectiveness? Especially for the clinician that does NOT have a strength training—or even exercise training—background. (Because it would be much different for that clinician, do you agree?)
Chuck: Absolutely I do. Many physical therapists don’t have backgrounds in strength and conditioning. For that reason, I have to be careful when I’m teaching physical therapists about kettlebells.
It’s not just a piece of cast-iron with a handle that athletes use at the CrossFit Games on ESPN. It’s a powerful and effective tool that can be used in the clinic to improve a patient’s strength and movement quality.
Once again, it goes back to the concepts I discussed. When I teach therapists the simplicity of the tool and how they can use it in the clinic, it changes everything. We have kettlebells in several of our clinics in my region. Just doing farmer’s walks alone is extremely safe for any physical therapist to teach their patients.
My physical therapists teach a lot of deadlifting patterns in the clinic. We can relate this back to a patient who is picking up a 40-pound bag of dog food, and now this can be accomplished in a safe and efficient manner.
Physical therapists in my clinics look for tension, hip hinging, and breathing. Did the patient reflexively brace? Did the patient engage the lats (anti-shrug) or did they shrug their shoulder?
The patient is taught how to properly lift using the basic movement concepts using the kettlebell to reinforce their functional movement patterns.
As a more seasoned therapist, I was taught lumbar stabilization techniques from the San Francisco Spine Center and it was a wonderful program. But, we never added load. That’s a problem.
Now we take lumbar stabilization using the kettlebell concepts and we’re adding loads using the kettlebell as the preferred tool. The bottom line is I can teach the simple 3 concepts mentioned earlier to any non-strength physical therapist today. They can walk away with that and can immediately help the patient. That’s powerful.
Scott: What’s the most important thing the clinician must learn before incorporating kettlebells?
Chuck: I think they need to become “clinically competent.” I’ll explain what I mean.
If you’re going teach a kettlebell exercises in the clinic, do you have competency with the kettlebell yourself? If you don’t truly understand the exercise yourself, you can’t promote it to the patient.

If a physical therapist doesn’t have clinical competency, they need to reach out to someone who has knowledge with kettlebells and make sure they have competency to teach their patients in a safe and effective manner.
Every physical therapist should have knowledge about the kettlebell concepts and fundamental exercises. Your patients should be able to pick up a 40-pound bag of dog food or their groceries in safe manner because you have taught your patients how to properly hinge from the hips, breathe, and create tension.
I was teaching a new physical therapy grad how to perform a kettlebell deadlift and the steps of the get-up. At the same time, I was also working with a student physical therapist who asked “why would I use that in the clinic?”
By the time our conversation had ended, the student—and the new physical therapist—understood the importance of the exercises. They understand how these simple concepts I keep talking about (hinge, breath, tension) could help a patient.
Clinical competency is about truly understanding full-body movement patterns with the tools they are teaching to their patients. It’s important.
Scott: To recap, what you’re saying is that the clinician should go and seek out a qualified, certified kettlebell instructor. They should obtain a baseline competency from someone that is skilled with using the tool before they would ever apply that in the clinical setting. Is that correct?
Chuck: Exactly. For example, it’s similar to when you need 100 hours of dry needling continuing education to become clinically competent to use that specific modality in the clinic.
Physical therapists need to search for people who are offering courses in strength training using kettlebells or other strength modalities in order to make sure they have the clinical competency to teach those concepts to their patients. This is critically important.
PTs are focused on evidence-based practice as a profession.
Unfortunately, physical therapy schools are not doing enough research in strength training to show the benefit of strength for the patients. As a regional manager for PIVOT Physical Therapy, I interview many doctorate physical therapists and, sadly most do not have much knowledge in strength training concepts.
Scott: Obviously, StrongFirst offers the one-day Kettlebell Course that teaches users entry-level kettlebell exercises and the principles of strength and movement. Do you agree that would be something that’s appropriate for the clinician who wants to bring kettlebells into the clinic?
Chuck: I do. I should also say that I took a one-day StrongFirst Bodyweight Course a few years ago. It was a foundational course on bodyweight exercises and I learned the basic concepts of tension with respect to bodyweight exercises. I was able to apply these concepts with patients upon returning to the clinic on Monday. I would advise all therapists to reach out and take the one-day StrongFirst Kettlebell Course to gain some clinical competency with the kettlebell.
In my career as a physical therapist, I have taken courses outside the physical therapy arena, which has changed the way I treat patients and train myself.
Some of the physical therapists in my region have embraced this concept and they have become the “Hybrid PTs” (hybrid physical therapist and strength-movement coaches). I’m 100% committed to getting patients moving better and stronger, as well as teaching more physical therapists to become these “Hybrid PTs” to improve their patients’ long-term outcomes.
Scott: Let’s talk about some examples of patients who aren’t in the ‘acute pain phase” of their program. What are some diagnoses that you’ve worked with and what type of patients have you seen benefit the most from using kettlebells?
Chuck: Chronic low back pain is very common in the outpatient physical therapy clinics.
As I tell my patients, “I’m not just the president of the low back pain club, I’m an active member.” I have a history of low-back pain since the 80’s, but using kettlebells to strengthen my posterior chain has been a game-changer in addressing my back issues.
Using the concepts (hinge, breath, and tension) has significantly changed my strength. Specifically, by using kettlebell swings, carries, and the get-up. Sharing these with patients, I’ve seen them gain strength and better movement patterns. I honestly don’t believe there is a better, more accessible strength tool out there than a kettlebell.
In the clinics, we will use kettlebell carries to get the patients to reflexively stabilize. Then progress to the bottom’s-up drills which have assisted in creating a more natural reflexive stability without “over-coaching” our patients.
The get-up is another incredible kettlebell exercise that we can use to improve patients’ mobility, stability, and durability. We break it down into the 7 steps for the patients as we progress the patients plan of care.
Many of our patients lack mobility in the thoracic spine; they have tight hip flexors, and they lack glute activation. These are common issues. In the get-up, we emphasize a high bridge and shoulder packing with the patients to help to correct these issues and more.
I couldn’t imagine seeing a patient today without somehow implementing variations of these 4 kettlebell exercises:
- Kettlebell Deadlifts
- Kettlebell Carries
- The Get-Up
- Overhead Press
Here’s a few additional insights I want to share.
Personal trainers and strength coaches should understand that when physical therapists are working with a patient, there is a scope of practice and laws they must follow.
Physical therapists are licensed practitioners and work with patients generally at very low levels of strength and muscle tissue (sarcopenia) with complex medical issues.
We may see the most challenged patients with respect to strength, mobility and general physical fitness. Most of the patients are uninformed, unmotivated, and are looking for a quick fix (meaning medications). But, let me say that getting strong is the best medicine in the world.
We, as physical therapists, have to be compliant with the government and state regulations. What I mean is that we can’t implement kettlebell exercises until we get the pain and inflammation under control. I have to gain the patient’s trust and confidence. I have to get them out of pain before using these tools. After that, I can hope to get unbelievable results.
Here’s a specific example. I was treating a patient referred to me by an orthopedic doc for shoulder tendonitis. The patient was a 17-year old baseball star pitcher from one of the local high schools.
Using an SFMA-based physical therapy evaluation, my assessment revealed that he had some notable motor control issues and tight hip flexors. He had no pain, but it was reproduced with his throwing. He had full range of motion and “special testing” revealed no positive findings. One component of my treatment approach for this patient was to teach him how to perform kettlebell deadlifts and get-ups to improve motor control and movement patterns.
He did the kettlebell exercises with zero pain. Then I got a phone call from the orthopedic doctor wanting to know why I wasn’t working his shoulder (why wasn’t doing typical external rotation work with Thera-bands).
It’s my fault for not sufficiently educating the orthopedic doctor, the patient, or his parents about my approach to the underlying cause of his shoulder issues. But once I explained the concepts and my plan of care, they were very satisfied. More importantly, the patient improved and had a successful senior season. Education is key, and this is a perfect example.
That’s one of the most challenging things when you are working with patients. You must make sure you’re educating both the patients—and the doctors—about what you’re doing and WHY. Doctors must trust that you’re going to do the best thing for their patients in a safe and effective manner.
As physical therapists, we must abide by our scope of practice and the laws. In addition, we have to change the perception of strength training with uninformed—and, potentially, unmotivated patients. Also keep in mind that if I had someone doing kettlebell exercises in the clinic and they got hurt, you bet there would be a lot of scrutiny and clinical review around that particular approach for the patient.
You have to be careful. You just can’t go “rogue” with physical therapy patients in the clinical setting using kettlebells.
Scott: Can you tell us about a specific kettlebell protocol you’ve used?
Chuck: I had a 54-year old right shoulder post-rotator cuff and labrum surgical repair. Following the doctor’s protocol and physiological healing principles, I was able to implement kettlebells into his rehab protocol.
Before we went into the strength training phase of his rehab, we began with some basic concepts that I’ve already discussed. We started with breathing to get the thoracic mobility restored. As you know, many people over 35 are going to present with restricted mobility in their thoracic spines. We started there.
In addition, we used Original Strength principles in the rehab process. The patient started with left-arm-only quadruped rocking, head control exercises, and rolls (using no arms). We eventually progressed to crawling.
We also started working on kettlebell presses on his unaffected side two weeks into his rehab. Why did we do this?
Because we’re getting the ‘irradiation’ carry-over for that client, which ties back to creating the ‘good tension’ thought the body. Obviously, we could not train the involved side because there’s a healing process going on there. But, going to the other side and using the irradiation process was huge.
Loaded carries and single arm deadlifts were added on the left (unaffected side) as we progressed the patient.
Four weeks into the rehab, we introduced sit-to-stand (box squats) for a functional isometric (the “Grip-Butt-Squeeze”) using the concepts of tension, hip hinge, and breathing.
At six weeks, we started with very light kettlebell pressing, tall-kneeling, then progressed to half-kneeling, and then finally to standing presses. Emphasis was placed on a tall spine, grip, and packing the shoulder (with an anti-shrug).
We followed the same approach with the various kettlebell carries, get-ups, mace-bells and Indian clubs.
It’s important to note that we also utilized some of the other standard physical therapy techniques and approaches (i.e., manual, range of motion, dry needling and other PT modalities).
Instead of using just Thera-band as our only tool of strengthening the shoulder/rotator cuff (we did do a little bit of that), we focused on the kettlebell, clubbells, macebells, and Indian clubs. We had tremendous results. Once again, we had to follow the protocol and we couldn’t deviate too far, but using the safe concepts really helped this client.
This 54-year old male (who weighs only 150 pounds) was pressing a 32kg kettlebell 12 months after a major surgery. That was quite impressive.
Scott: What are your thoughts and experiences with swings? Do you use them and are they appropriate in the clinical setting?
Chuck: Yes, but only for the right patient and diagnosis. First, you need to consider their fitness level and strength background.
We’ll get a lot of CrossFit folks who like to do the American-style swings, but without the ability to properly hinge at the hips or lock out at the top of the swing. We show them how to do a proper hip hinge pattern and how to lock out the hips for a proper hardstyle swing.
We’re going to see these type of patients in the clinics with the rise of CrossFit boxes in our region. They are being referred to us for lumbar strains, so we have to know a proper kettlebell swing technique to have credibility with that type of patient.
The wrong approach would be to say it’s unsafe to swing kettlebells and you should quit going to your CrossFit gym. That doesn’t solve the problem.
We also see athletes and weekend warriors who “squat swing” the kettlebell. They hear about kettlebell benefits from a personal trainer at a big box gym, a friend, or sports coach. But, most of them have not been properly trained and that’s when they get hurt.
We even see patients who have learned how to swing a kettlebell from a poorly-instructed fitness DVD, which is unfortunate. They’re so grateful because we can show them how to correctly swing the kettlebell and their back and knees don’t hurt anymore. Their power production increases and it’s a whole new world for them. It’s pretty amazing.
Scott: Let’s close this with the specific next steps for the clinician looking to use kettlebells in the clinical setting. What are the key things they absolutely must do or consider?
Chuck: Finding a certified kettlebell instructor in your local area is a great place to start.
Consider the StrongFirst Kettlebell Course to be educated in basics and become clinically competent.
Get around like-minded people and start training with a kettlebell the right way. To me, if you want to be a great clinician, you’re always learning and trying to improve your game.
If I looked back at what I did 22 years ago as a therapist and what I thought I knew about the strength game compared to what I know today, there’s only one reason that I know so much more.
It’s because I didn’t sit back and accept the “status quo.” I kept getting in the game and learning. You have to do that.
Physical therapists are doctorates now. But, the strength training concepts and understanding, they aren’t there yet.
As clinicians, we understand the science part very well. But, like anything, you have to actually experience what it feels like to swing a kettlebell or perform a get up. You can just learn the theory, you actually have to practice.
Reach out to people and keep asking questions like how do we get patients stronger? And, understand why.
At the end of the day, that’s what we’re here for. To get our patients moving better and getting them stronger to restore function and prevent injury from happening in the first place.

Summary Points
If you’re a clinician and are considering using kettlebells in the clinical setting, here’s a concise recap for the next steps.
1. Find a local certified instructor to learn from. Learn about kettlebells, movement, and strength principles with “live-in-person” training to accelerate your understanding about the proper use and applications of kettlebells.
2. Consider taking a StrongFirst Kettlebell Course. It’s one day, 8-hour immersion into the basic concepts and principles of kettlebell applications. This is an intelligent investment in understanding strength and movement.
3. Although not mentioned in this discussion, it’s highly recommended to read Kettlebell Simple and Sinister by Pavel. This book provides core understandings about the kettlebell fundamentals and principles.
4. Take the StrongFirst For Clinicians Course. This is a new course specifically designed to help clinicians understand the powerful role of strength in the rehab setting. Clinicians will learn specific principles and foundational applications of kettlebell and barbell training for their patients. The next course takes place August 4-5 in Denver, Colorado.
____________________________________
Scott Iardella, MPT, CSCS, SFG II, SFL, CISSN, USAW, CACWC: Scott’s bio is below.
Chuck Mutschler, MPT, MS, CSCS, SFMA, FMS, OS Certified Clinician: Chuck is currently a Regional Manager for Pivot Physical Therapy in Southern Maryland. He earned his Master’s Degree in Physical Therapy from the University of Maryland School of Medicine and went on to own multiple physical therapy clinics in Anne Arundel and Howard County in Maryland. His passion for strength and conditioning led to advanced certifications as a CSCS from the National Strength and Conditioning Association, SFG Level II Instructor from the StrongFirst School of Strength, OS Certified Clinician from Original Strength Systems, SFMA and FMS form Functional Movement Systems. Chuck has been a guest lecturer throughout the mid-Atlantic region, discussing topics such as Orthopedic Physical Therapy, Kettlebell Training, Corrective exercises, Fall Prevention, Primitive Movement Patterns, Circular Strength Training and Sports Medicine.








As a PT who has been training w KB’s for about 5 years, I agree with all of the above; the main difference is that I work with pediatric population and can tell you that I’ve done deadlifts, carries and parts of the get up (without a bell) with kids as young as 3 years old, and they are a fantastic tool not only in terms of strengthening, but just from a baseline developmental as well as sensory integration perspective.
Great conversation Scott and Chuck!